HL7 and FHIR are industry-standard protocols enabling secure and structured EHR data exchange.
HL7 remains the backbone of many legacy healthcare systems, while FHIR introduces modern, API-driven integration.
Standards reduce errors, improve patient safety, and enhance interoperability between providers, apps, and systems.
Common challenges include inconsistent implementations, terminology mismatches, and legacy system constraints.
Platforms like eZintegrations™ and Goldfinch AI help overcome these barriers through AI-based automation and no-code interfaces.
Electronic Health Records (EHRs) are the central hub of patient care, but their value is limited if systems can’t communicate. Despite massive adoption (94%+ among US hospitals), data exchange across providers remains fragmented. HL7 and FHIR standards aim to solve this by enabling a common language for health data across apps, organizations, and geographies.
As regulations such as the 21st Century Cures Act mandate API access and interoperability, healthcare organizations must adopt HL7 and FHIR to remain compliant, improve patient outcomes, and drive operational efficiency.
HL7 (Health Level Seven) is a set of international standards that define how health data is structured and shared electronically. It’s the backbone for many hospital and lab systems. It is a long-standing set of international standards that helps healthcare systems communicate clinical and administrative data electronically.
It’s especially useful in traditional EHR environments that rely on message-based exchanges. Even though newer standards like FHIR are emerging, HL7 remains vital in many hospitals and labs due to its wide adoption and reliability.
Message-based (like HL7 v2, v3)
Suitable for lab results, billing, admission/discharge, and radiology
Still widely used in hospitals for clinical workflows
XML-based formats like CDA (Clinical Document Architecture)
While HL7 is mature and stable, it has limitations in modern app-based environments due to its complexity and lack of real-time data access.
FHIR (Fast Healthcare Interoperability Resources) is HL7’s modern standard. Designed with developers in mind, FHIR uses REST APIs, JSON/XML data formats, and modular resources to make healthcare integration more flexible, scalable, and web friendly.
is the next-gen standard developed by HL7 to simplify health data exchange using web technologies. It enables real-time, app-friendly communication between systems and offers a modular, resource-based format that’s easy for developers to use. FHIR adoption is growing rapidly due to its alignment with digital transformation and regulatory mandates.
Real-time access via RESTful APIs
Standardized resources for patient, lab, medication, appointments, etc.
Easier adoption by mobile, web, and cloud-based apps
Interoperability with SMART on FHIR apps and 3rd party platforms
FHIR adoption is accelerating, with most major EHR vendors offering FHIR endpoints.
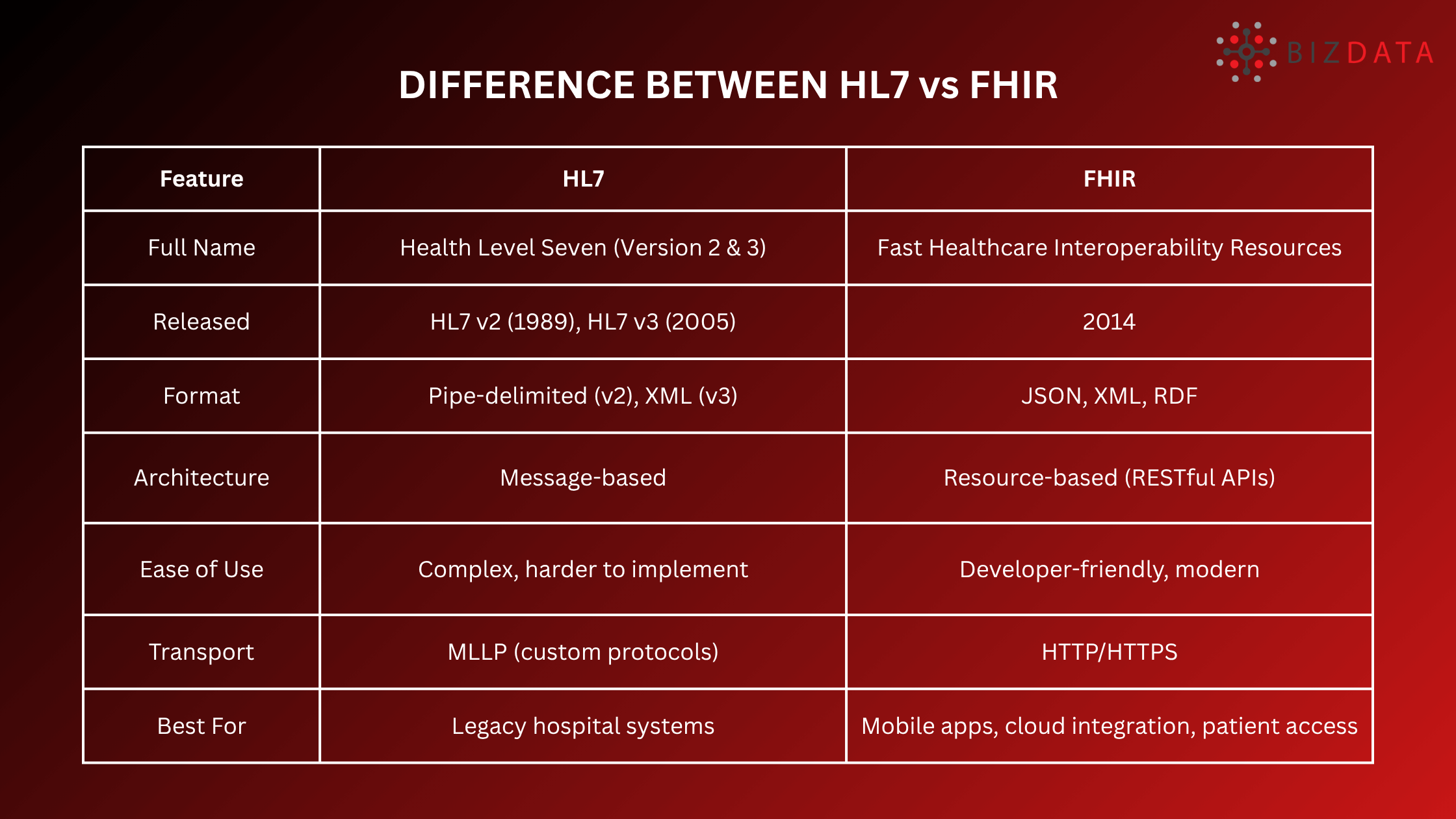
Although both HL7 and FHIR aim to improve interoperability, they serve different use cases. HL7 works best for legacy systems and internal data flows, while FHIR supports modern, API-first ecosystems.
Understanding the difference helps organizations plan hybrid integration strategies that bridge old and new technologies effectively. Use HL7 for legacy system compatibility and FHIR for modern app-based workflows.
In B2B healthcare environments like between hospitals, labs, insurers, and digital health platforms standards:
Enable scalable integration across disparate systems and partners
Reduce risk of data loss or misinterpretation
Support regulatory mandates like TEFCA and Cures Act compliance
Accelerate time-to-market for healthcare SaaS vendors and EHR-connected solutions
Also Check out: Top Best Healthcare Interoperability Solutions: Guide for 2026
Healthcare Data Integration: AI Guide & Best Practices 2026
EHR Integration: Ultimate Guide 2026
Adopting HL7 and FHIR standards brings significant benefits in both clinical and business settings. They make data exchange safer, faster, and more standardized, improving outcomes and enabling innovation. These protocols ensure that EHR systems work cohesively, regardless of vendor or deployment model.
Before diving into best practices, it’s important to recognize the core benefits that standards-based integration brings to healthcare enterprises:
Data Accuracy: Standardized vocabularies reduce human and system errors.
Interoperability: Ensures seamless communication between labs, hospitals, payers, and apps.
Regulatory Compliance: Simplifies adherence to HIPAA, ONC, and FDA mandates.
Speed & Scalability: API-based models scale across cloud apps and devices.
Innovation Readiness: Enables AI, telehealth, and wearable integrations faster.
Even with standards like HL7 and FHIR, integration isn’t plug-and-play. Healthcare systems often face version mismatches, incomplete implementations, and conflicting terminologies. These issues can slow down projects and require additional tools or expertise to resolve.
Even with standards, real-world integration is complex. Challenges include:
Version inconsistencies (e.g., FHIR R4 vs R5)
Custom data models by different EHR vendors
Mapping legacy fields to FHIR resources
Security and consent management
Limited resources in smaller IT teams
To get the most out of HL7 and FHIR, organizations should follow integration best practices. These include clearly defining data needs, using API management layers, and validating terminologies. A strategic and phased approach reduces risk and helps scale integration projects smoothly.
To overcome the challenges and ensure successful implementation, healthcare tech teams should:
Define Your Integration Scope: Clarify which systems (EHRs, LIS, RIS, etc.) need to talk.
Choose the Right Standard(s): Use HL7 for legacy systems and FHIR for cloud-native or real-time data.
Validate Terminologies: Use SNOMED CT, LOINC, and RxNorm for clinical concepts.
Leverage API Gateways: For security, access control, and throttling.
Pilot Before Full Deployment: Validate mappings and workflows before scaling.
Modern platforms use AI to:
Auto-map unstructured documents (scans, PDFs) into structured FHIR data
Predict anomalies in real-time data streams
Translate non-standard legacy data into interoperable formats
Automate test case generation for validation
Goldfinch AI, for instance, can parse referrals, handwritten documents, and older EMR records into standardized data without manual effort cutting integration time drastically.
Telemedicine Apps using FHIR to pull allergies, meds, and lab results directly from Epic or Cerner.
Insurance Platforms using HL7 for eligibility verification and claims tracking.
Health Exchanges (HIEs) using hybrid HL7 and FHIR to support multi-provider networks.
AI Analytics Vendors using FHIR for real-time access to clinical data lakes.
Looking ahead, expect:
FHIR R5 and beyond: More mature capabilities for decision support, scheduling, billing
FHIR SQL: Transforming APIs into queryable data lakes
Voice-based healthcare apps using FHIR backends
Blockchain + FHIR: For consent and immutable audit trails
Cross-border Interoperability via SMART Global APIs and TEFCA frameworks
eZintegrations™ is a no-code integration platform with:
Pre-built connectors for HL7, FHIR, EHRs, labs, and APIs
Drag-and-drop pipelines
Built-in mapping and error handling
Real-time data sync
Goldfinch AI complements this with:
AI-powered document parsing (e.g., lab results, claims)
NLP-based content extraction for FHIR bundling
OCR-to-FHIR transformation for scanned data
Together, they offer one of the most complete EMR/EHR integration stacks without writing code.
HL7 and FHIR are essential for modern healthcare data exchange. They provide the structure, security, and scalability required to unify fragmented healthcare ecosystems.
By pairing these standards with powerful platforms like eZintegrations™ and Goldfinch AI, healthcare providers, payers, and SaaS vendors can accelerate time-to-value, ensure compliance, and drive better outcomes.
Ready to streamline your EHR integration?
Book your free demo of eZintegrations™ today and experience seamless, standards-based interoperability powered by no-code AI.
Q1: Can HL7 and FHIR coexist?
Yes. Most real-world integrations use HL7 v2 for legacy systems and FHIR for modern APIs.
Q2: Do all EHRs support FHIR?
Most major EHR vendors like Epic, Cerner, and Allscripts now expose FHIR endpoints, though with vendor-specific nuances.
Q3: Is FHIR open-source?
Yes, the FHIR standard is publicly available and maintained by HL7.
Q4: What is SMART on FHIR?
A framework for building secure, pluggable apps that use FHIR APIs and OAuth2 for access.
Q5: How do I ensure FHIR compliance?
Use FHIR validators, conformance testing tools, and middleware like eZintegrations™ to abstract complexity.